What is Borderline Personality Disorder?
Borderline personality disorder is an illness marked by an ongoing pattern of varying moods, self-image, and behavior. These symptoms often result in impulsive actions and problems in relationships with other people. A person with borderline personality disorder may experience episodes of anger, depression, and anxiety that may last from a few hours to days. Recognizable symptoms typically show up during adolescence. or early adulthood, but early symptoms of the illness can occur during childhood.
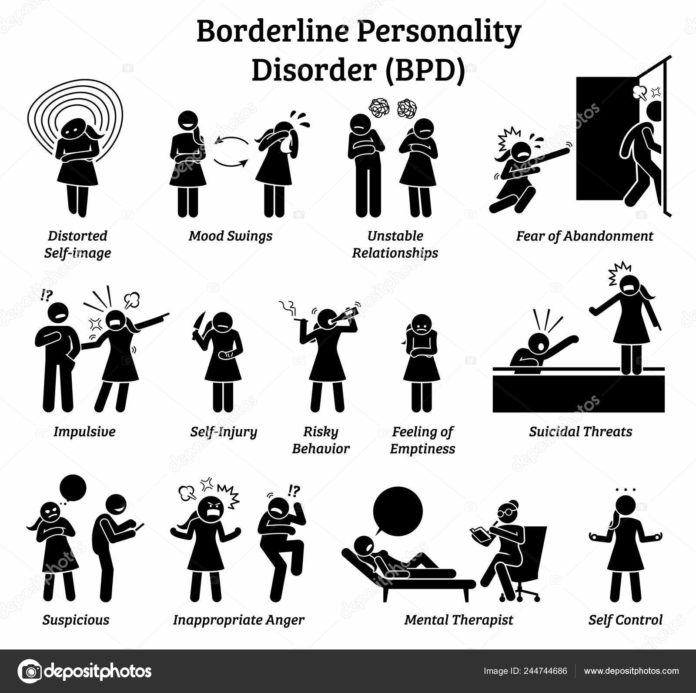
What are the signs and symptoms?
People with borderline personality disorder may experience mood swings and may display uncertainty about how they see themselves and their role in the world. As a result, their interests and values can change quickly. People with borderline personality disorder also tend to view things in extremes, such as all good or all bad. Their opinions of other people can also change quickly. An individual who is seen as a friend one day may be considered an enemy or traitor the next. These shifting feelings can lead to intense and unstable relationships.
Other signs or symptoms may include:
- Efforts to avoid real or imagined abandonment, such as rapidly initiating intimate (physical or emotional) relationships or cutting off communication with someone in anticipation of being abandoned
- A pattern of intense and unstable relationships with family, friends, and loved ones, often swinging from extreme closeness and love (idealization) to extreme dislike or anger (devaluation)
- Distorted and unstable self-image or sense of self
- Impulsive and often dangerous behaviors, such as spending sprees, unsafe sex, substance abuse, reckless driving, and binge eating. Please note: If these behaviors occur primarily during times of elevated mood or energy, they may be indicative of a mood disorder, rather than borderline personality disorder.
- Self-harming behavior, such as cutting
- Recurring thoughts of suicidal behaviors or threats
- Intense and highly changeable moods, with each episode lasting from a few hours to a few days
- Chronic feelings of emptiness
- Inappropriate, intense anger or problems controlling anger
- Difficulty trusting, which is sometimes accompanied by irrational fear of other people’s intentions
- Feelings of dissociation, such as feeling cut off from oneself, observing oneself from outside one’s body, or feelings of unreality
Not everyone with borderline personality disorder experiences every symptom. Some individuals experience only a few symptoms, while others have many. Symptoms can be triggered by seemingly ordinary events; for example, people with borderline personality disorder may become angry and distressed over minor separations — due to business trips or changes in plans — from people to whom they feel close. The severity and frequency of symptoms and how long they last will vary depending on the individual and their particular illness.
What causes borderline personality disorder?
Scientists aren’t sure what causes borderline personality disorder, but research suggests that genetic, environmental, and social factors play a role.
- Family History. People who have a close family member (such as a parent or sibling) with the disorder may be at a higher risk of developing borderline personality disorder or borderline personality disorder traits (such as impulsiveness and aggression).
- Brain Factors. Studies show that people with borderline personality disorder can have structural and functional changes in the brain especially in the areas that control impulses and emotional regulation. But is it not clear whether these changes were risk factors for the disorder, or caused by the disorder.
- Environmental, Cultural, and Social Factors. Many people with borderline personality disorder report experiencing traumatic life events, such as abuse, abandonment, or adversity during childhood. Others may have been exposed to unstable, invalidating relationships, and hostile conflicts.
Although these factors may increase a person’s risk, it does not mean that the person will develop borderline personality disorder. Likewise, there may be people without these risk factors who will develop borderline personality disorder in their lifetime.
How do I know if I have borderline personality disorder?
A licensed mental health professional—such as a psychiatrist, psychologist, or clinical social worker—experienced in diagnosing and treating mental disorders can diagnose borderline personality disorder, based on a thorough interview and a discussion about symptoms. A careful and thorough medical exam can also help rule out other possible causes of symptoms.
The mental health professional may ask about symptoms and personal and family medical histories, including any history of mental illness. This information can help determine the best treatment.
What other illnesses often co-occur with borderline personality disorder?
Borderline personality disorder often occurs with other mental illnesses. These co-occurring disorders can make it harder to diagnose and treat borderline personality disorder, especially if symptoms of other illnesses overlap with the symptoms of borderline personality disorder. For example, a person with borderline personality disorder may be more likely to also experience symptoms of major depression, bipolar disorder, anxiety disorders, substance abuse, or eating disorders.
How is borderline personality disorder treated?
Borderline personality disorder has historically been viewed as difficult to treat. But with newer, evidence-based treatment, many people with borderline personality disorder experience fewer and less severe symptoms, improved functioning, and an improved quality of life. It is important for patients with borderline personality disorder to receive evidence-based, specialized treatment from an appropriately-trained mental health professional. Other types of treatment, or treatment provided by a provider who is not appropriately trained, may not benefit the patient.
Many factors affect the length of time it takes for symptoms to improve once treatment begins, so it is important for people with borderline personality disorder and their loved ones to be patient and to receive appropriate support during treatment.
It is important to seek—and stick with—treatment.
NIMH-funded studies indicate that borderline personality disorder patients who don’t receive adequate treatment are more likely to develop other chronic medical or mental illnesses and are less likely to make healthy lifestyle choices. Borderline personality disorder is also associated with a significantly higher rate of self-harm and suicidal behavior than the general population.
Suicide and Self-Harming Behaviors
Borderline personality disorder is associated with higher rates of suicide and self-harming behaviors. Patients with borderline personality disorder who are thinking of harming themselves or attempting suicide need help right away.
Psychotherapy
Psychotherapy is the first-line treatment for people with borderline personality disorder. It can be provided one-on-one between the therapist and the patient or in a group setting. Therapist-led group sessions may help teach people with borderline personality disorder how to interact with others and how to express themselves effectively. It is important that people in therapy get along with and trust their therapist. The very nature of borderline personality disorder can make it difficult for people with this disorder to maintain a comfortable and trusting bond with their therapist.
Two examples of psychotherapies used to treat borderline personality disorder include Dialectical Behavior Therapy (DBT) and Cognitive Behavioral Therapy (CBT).
DBT, which was developed for individuals with borderline personality disorder, uses concepts of mindfulness and acceptance or being aware of and attentive to the current situation and emotional state. DBT also teaches skills to control intense emotions, reduce self-destructive behaviors, and improve relationships.
CBT can help people with borderline personality disorder identify and change core beliefs and behaviors that underlie inaccurate perceptions of themselves and others and problems interacting with others. CBT may help reduce a range of mood and anxiety symptoms and reduce the number of suicidal or self-harming behaviors.
Medications
Medications are not typically used as the primary treatment for borderline personality disorder as the benefits are unclear. However, in some cases, a psychiatrist may recommend medications to treat specific symptoms, such as mood swings, depression, or other mental disorders that may occur with borderline personality disorder. Treatment with medications may require care from more than one medical professional.
Certain medications can cause different side effects in different people. Individuals should talk to his or her provider about what to expect from a particular medication.
Other Elements of Care
Some people with borderline personality disorder experience severe symptoms and require intensive, often inpatient, care. Other people may need outpatient treatments but never need hospitalization or emergency care.